What is Periodontal (or Gum) Disease?
Periodontal (or gum) disease is a chronic disease, much like diabetes and cardiovascular disease, that causes destruction to gums and bone. Periodontal disease is essentially an infection of the gums. The infection must be treated and eliminated to avoid bone, tissue, and tooth loss, among other problems. In fact, gum disease, left unchecked, may exacerbate and lead to increased risks of heart disease, certain forms of cancer, respiratory disease, stroke, as well as other diseases and medical conditions.
A study published in the Journal of the American Dental Association found that nearly 50% of adults over 30 are affected by periodontal disease. It’s important for patients to be aware that there is no cure for gum disease. Gum disease can only be managed and requires constant monitoring to ensure that it does not progress any further and cause more destruction to a patient’s gums and bone.
What Causes Periodontal Disease?
Periodontal disease is caused by a sticky film of bacteria, called plaque, which is always forming on your teeth. When a patient fails to keep up with regular dental visits, the bacteria in plaque will cause gums to become inflamed, which then causes gums to pull away from teeth creating spaces called “pockets.” Plaque gets trapped in these pockets and cannot be removed by regular brushing at home, and can only be removed by your dentist.
Other reasons that may cause periodontal disease include
- poor dental hygiene
- smoking
- aging
- changes in hormones
- poor nutrition
- family history
- other medical conditions
What Are Symptoms of Periodontal Disease And What Can Happen If It’s Not Treated?
Deep pockets between gums and teeth are a common symptom of periodontal disease. Other symptoms include:
- bleeding gums
- inflamed, red, or tender gums
- bad breath
- receding gums
- shifting permanent teeth
- a change in your bite.
Left untreated, periodontal disease can and will lead to:
- bone and tissue loss
- tooth loss
- loose teeth
- moving teeth
It’s also important to note that the loss of bone and tissue can affect a patient’s tooth replacement options in the future. Bone and tissue are vital for replacement options such as crowns, bridges, and implants. When periodontal disease is left untreated, tooth loss can occur and when tooth loss occurs, so does bone and tissue loss. Depending on how much bone and tissue is lost, replacement options such as crowns, bridges, and implants may no longer be an option.
How Is Periodontal Disease Treated?
Periodontal disease is treated by three procedures, completed one after the other. The first procedure is called scaling and root planing, which is commonly known as a deep cleaning. However, scaling and root planing is much more in-depth than a typical cleaning and requires local anesthetic as the dentist goes underneath the gum line to remove plaque and tartar.
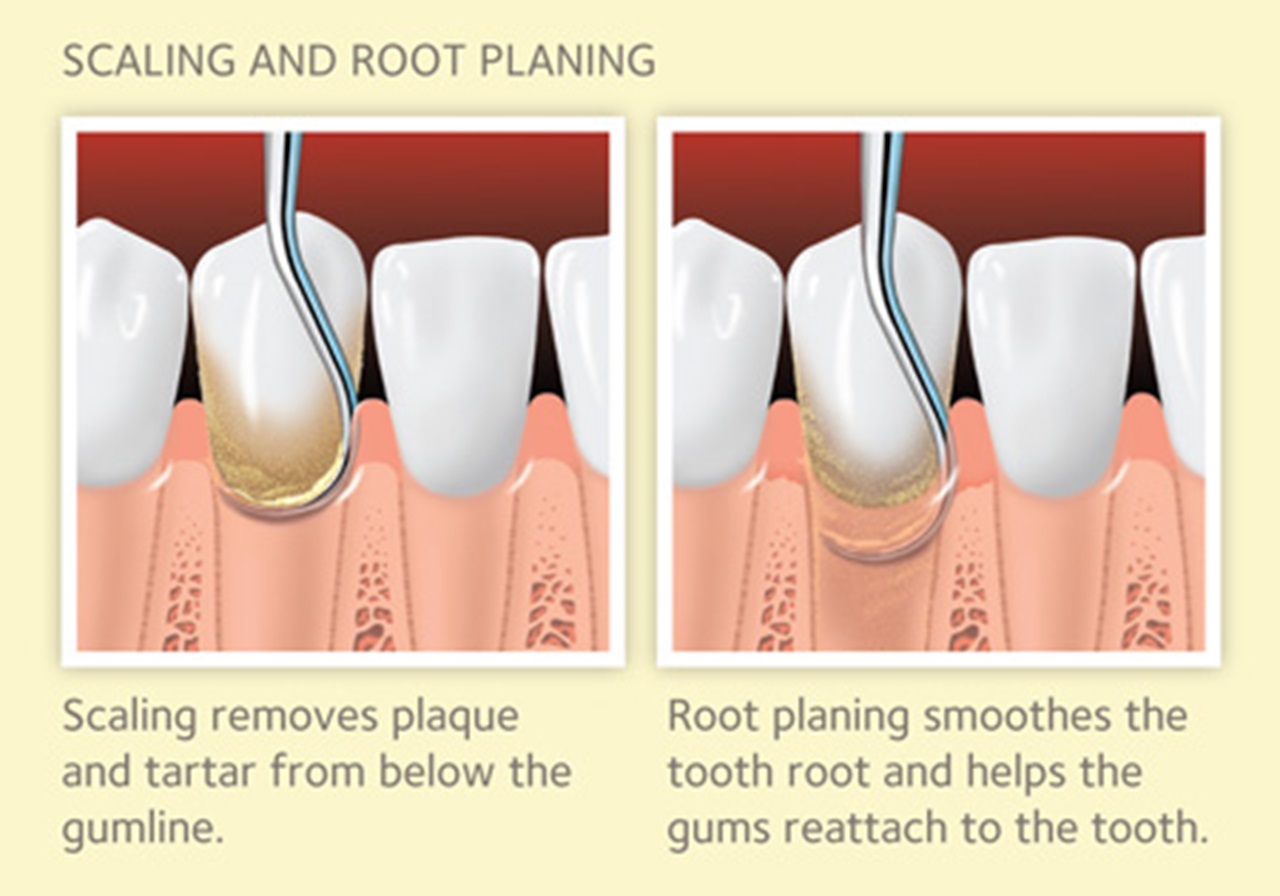
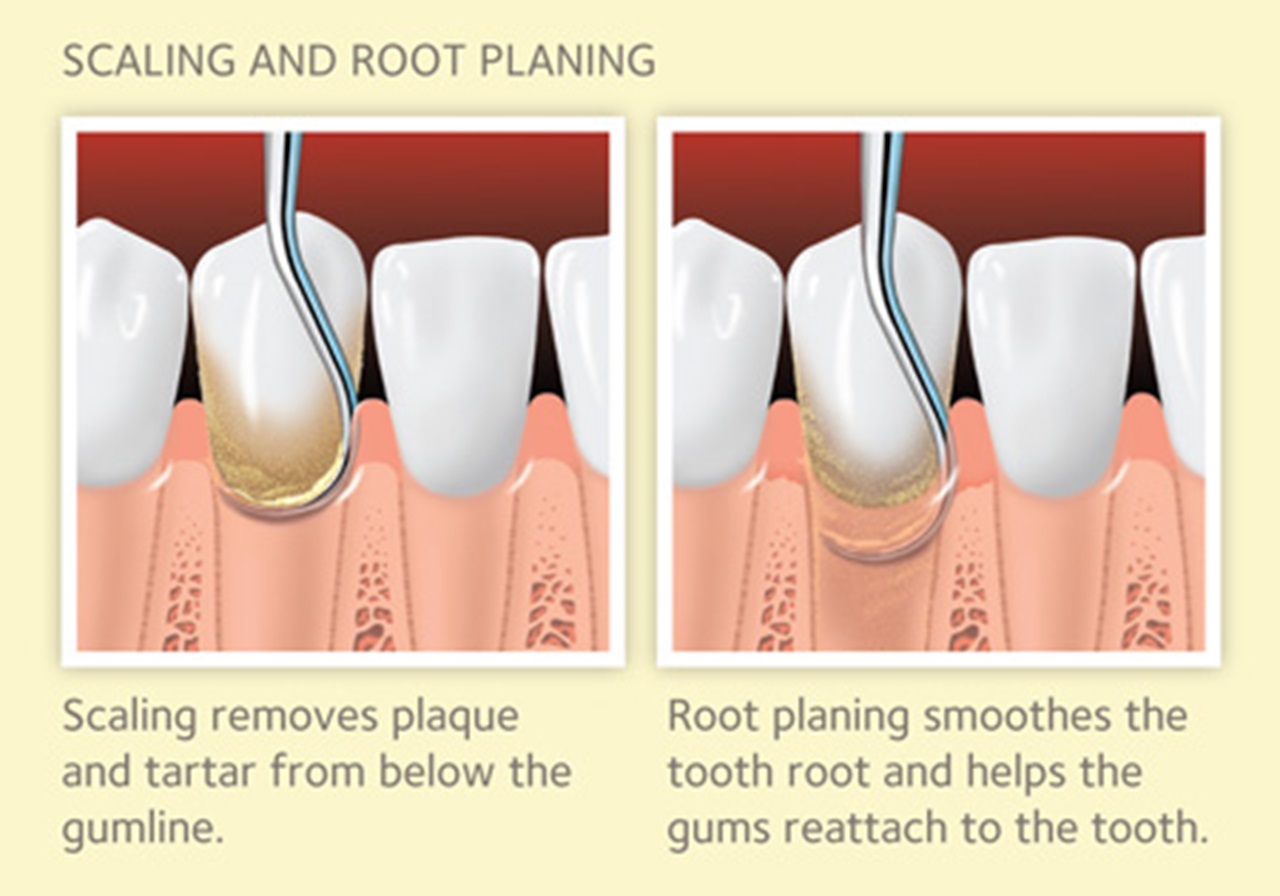
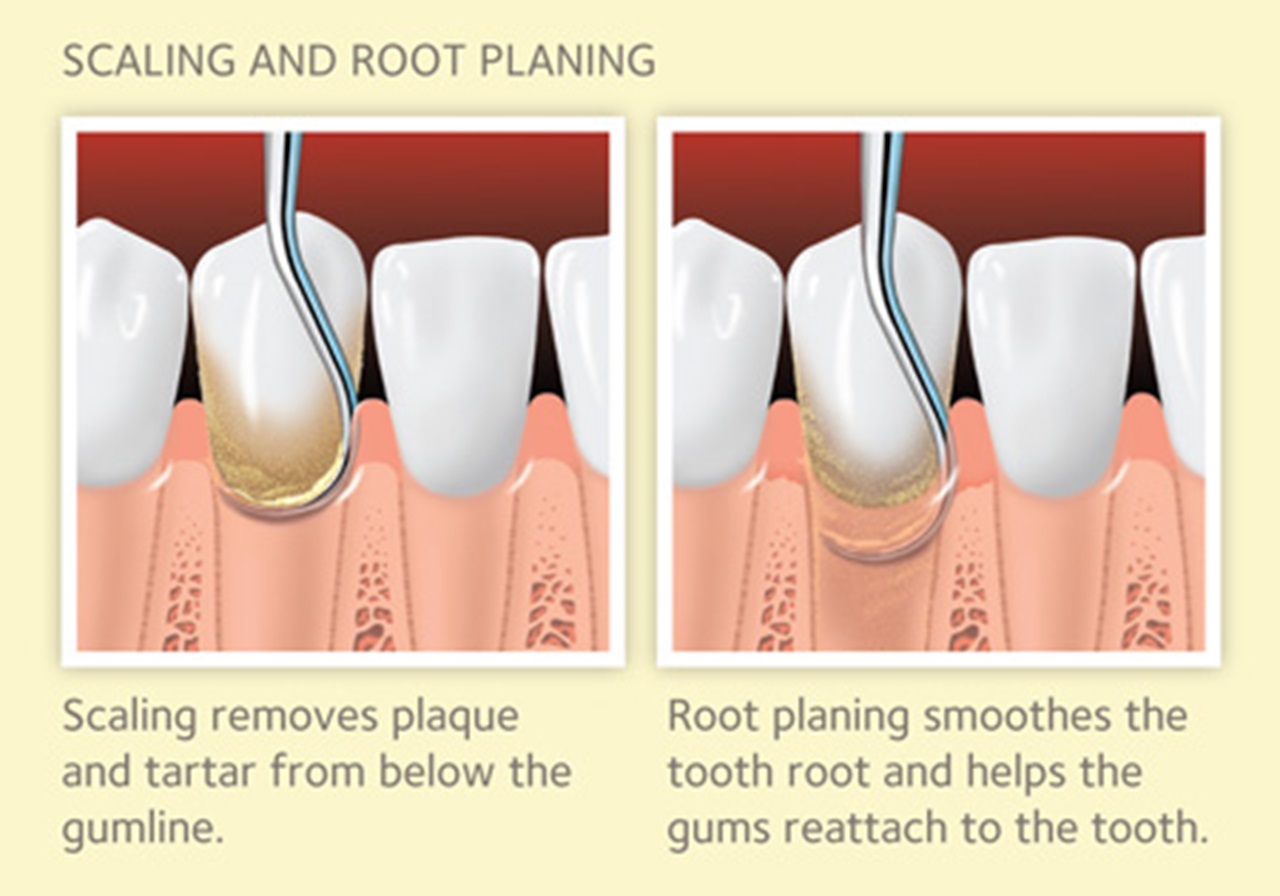
Periodontal scaling involves scraping the plaque and tarter from your teeth, below your gumline, and in any large pockets that have developed between your teeth and gums. Your dentist will then conduct root planing, a process where the dentist will smooth the tooth roots underneath your gumline using a scaling tool. This smoothing helps your gums to reattach to your teeth.
The second procedure is called gingival irrigation. This is done after scaling and root planing. During this procedure, the dentist uses an antimicrobial rinse to flush out the periodontal pockets. The antimicrobial rinse also works to eliminate harmful bacteria from underneath the gum line (the same bacteria that causes bone, tissue, and tooth loss).
The last procedure is called laser-assisted periodontal therapy. This is the final procedure used to treat periodontal disease, and is done after gingival irrigation. During this procedure, the dentist uses a soft-tissue diode laser to destroy 100% of the harmful bacterial underneath the gum line. The laser therapy also removes diseased tissue to allow for healthier gum tissue to regrow. During laser-assisted periodontal therapy, the dentist reshapes the patient’s gums by eliminating periodontal pockets, and in doing so, ensures that a patient’s gums are sealed to their teeth. By ensuring that the seal between a patient’s gums and teeth are intact, the patient is able to avoid further periodontal problems in the future, such as bone, tissue, and tooth loss.
After Periodontal Disease is Treated, What Are the Next Steps? The Importance of Periodontal Maintenance
It’s important to remember that periodontal disease is a chronic disease. Just like diseases like heart disease and diabetes, there is no cure for periodontal disease. Periodontal disease can only be managed and it requires constant monitoring by your dentist to ensure that the gum disease does not progress further and cause further destruction to gums and bone.
After periodontal treatment, harmful bacteria that leads to periodontal disease is eliminated. However, because a person is always eating food, bacteria is constantly reintroduced into the mouth. Bacteria reproduces rapidly and can return to destructive levels in as few as 90 days. This is the same harmful bacteria that leads to bone, tissue, and tooth loss.
To avoid destructive levels of harmful bacteria, gum disease is “maintained” by regular periodontal maintenance care visits. Regular periodontal maintenance visits every 3 months are extremely important for maintaining the health of your gums to minimize any further bone and tissue loss. Without regular periodontal maintenance visits, destructive levels of bacteria will exacerbate gum disease to severe levels and lead to bone, tissue, and tooth loss.
However, it is not just bone, tissue, and tooth loss – left unchecked, gum disease may also exacerbate and lead to increased risks of heart disease, certain forms of cancer, respiratory disease, stroke, as well as other diseases and medical conditions.